Chronic Obstructive Pulmonary Disease (COPD) is an umbrella term used to describe progressive lung diseases including emphysema, chronic bronchitis, and refractory (non-reversible) asthma. This disease is characterized by increasing breathlessness. COPD is a progressive and (currently) incurable disease, but with the right diagnosis and treatment, there are many things you can do to manage your COPD and breathe better. People can live for many years with COPD and enjoy life.
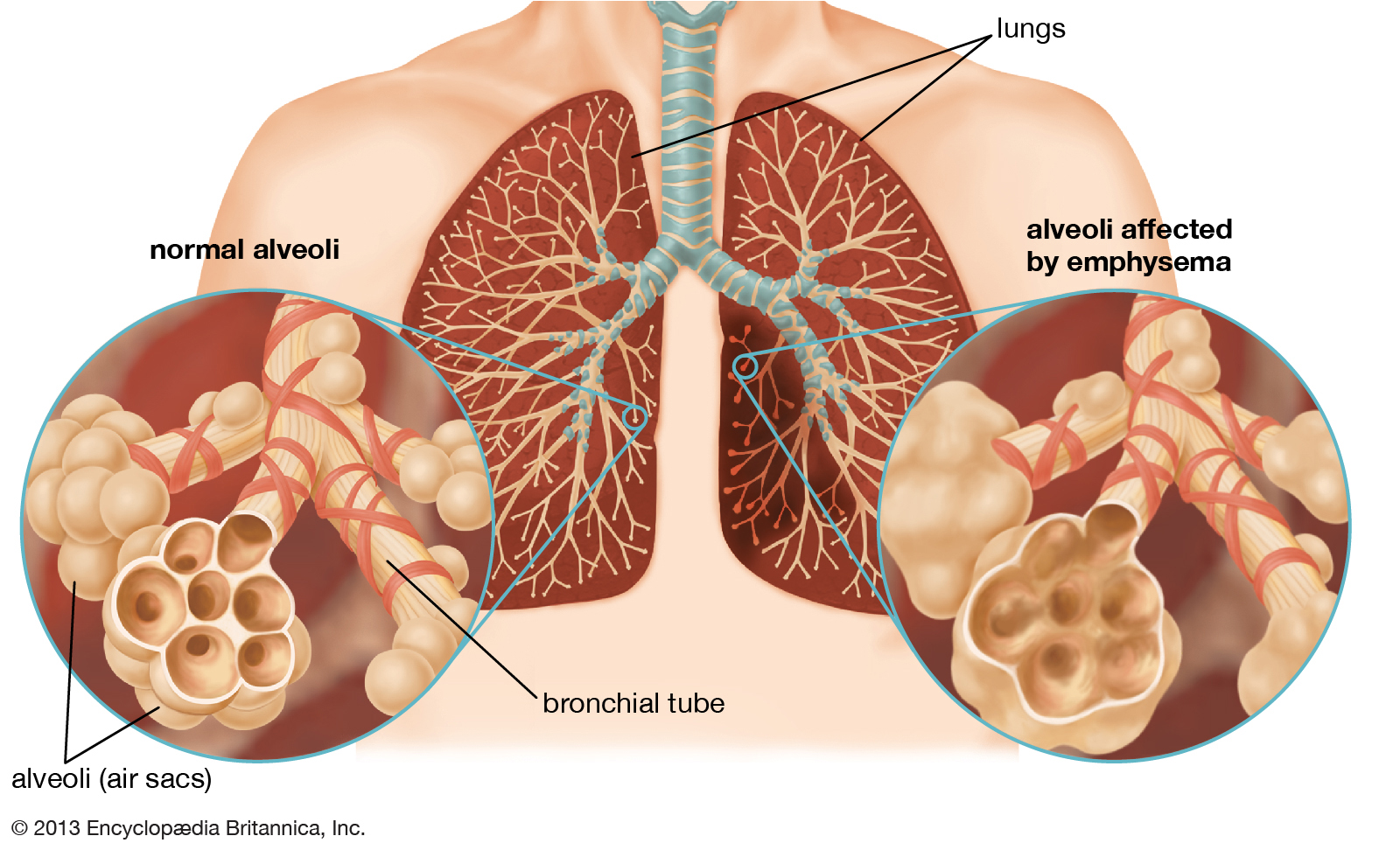
Emphysema
Damage to the alveoli (air sacs) causes emphysema. The walls inside the alveoli disappear, making many small sacs become larger, single sacs. These larger sacs do not absorb oxygen as well. So, less oxygen is absorbed into the blood. Also, when the alveoli are damaged, the lungs become stretched out and lose their springiness. The airways become flabby, and air is trapped in the lungs. It becomes hard to breathe out. This creates a feeling of shortness of breath.
Chronic Bronchitis
Damage to the bronchial tubes causes chronic bronchitis. Bronchitis occurs when the bronchial tubes are irritated and swollen. This causes coughing and shortness of breath. If mucus comes up with the cough and the cough lasts at least three months for two years in a row, the bronchitis has become chronic bronchitis.
There are hair-like fibers lining the bronchial tubes of the lungs. These tiny hairs are called cilia. The cilia help move mucus up the tubes so it can be coughed out. In chronic bronchitis, the tubes have lost their cilia. This makes it hard to cough up mucus, which causes more coughing. More coughing makes the tubes more irritated. This creates more mucus. The tubes then become swollen, making it hard to breathe. Smoking even just a little keeps the cilia from working normally. Mucus can build up in the lungs. This can cause more damage.
Refractory (non-reversible) asthma
Refractory (non-reversible) asthma is a type of asthma that does not respond to usual asthma medications. In an asthma attack, bronchial airways tighten up and swell. Medications can usually reverse this, opening up the airways and returning them to how they were before the asthma attack. In refractory asthma, medications cannot reverse the tightening and swelling of the airways.